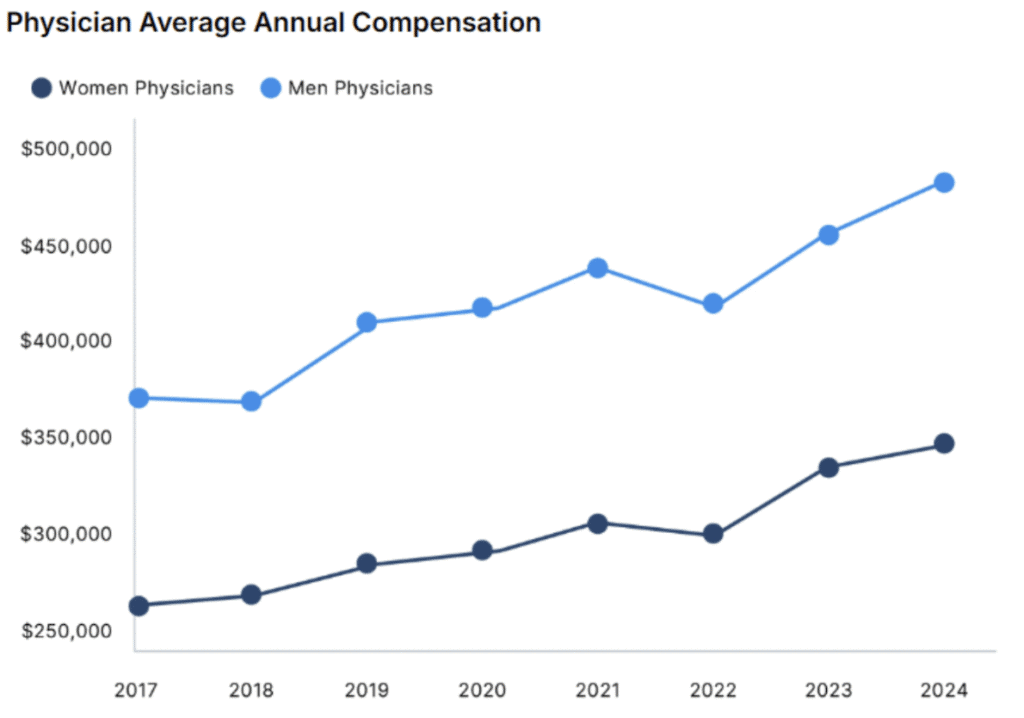
The latest Doximity compensation report reveals a physician workforce under mounting pressure. While average pay increased 3.7% from 2023 to 2024, this modest bump tells only part of the story.
Behind these numbers lies a profession grappling with widening pay gaps, declining reimbursement, and a compensation structure that appears increasingly misaligned with the realities of modern medical practice.
The Big Picture: Growth Slowing
Based on responses from over 37,000 physicians, average compensation now stands at roughly $425,000 across specialties. This represents a slowdown from the 5.9% growth reported the previous year.
When you factor in Medicare payment cuts and several years of elevated inflation, real purchasing power has barely budged for many physicians.
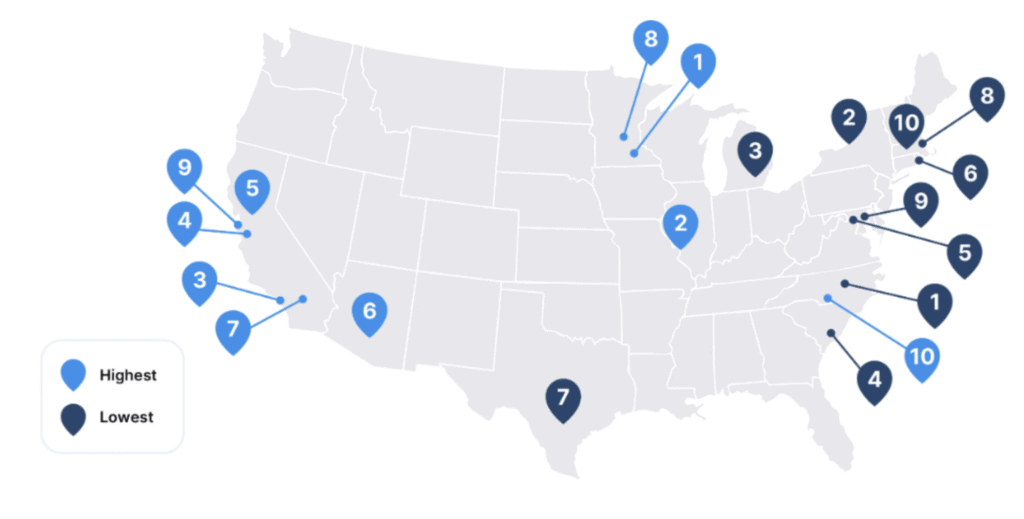
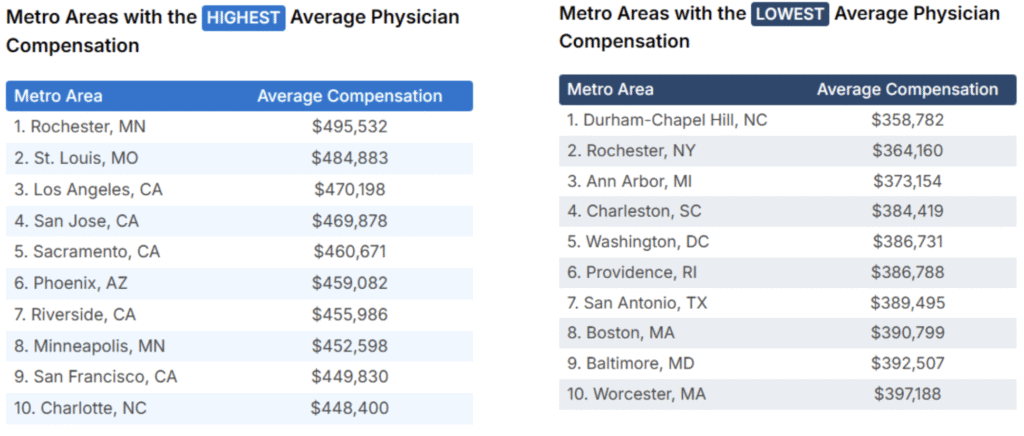
The geographic spread remains substantial. Rochester, Minnesota, tops the list at $495,532, anchored by the Mayo Clinic’s outsized presence in a small market. Five of the top ten highest-paying metros sit in California, despite the state’s high cost of living. On the other end, Durham-Chapel Hill comes in lowest at $358,782, followed by Rochester, New York, and Ann Arbor, Michigan.
When adjusted for cost of living, the picture shifts considerably.
Rochester, Minnesota maintains its top position, while Boston and Washington, D.C. occupy the bottom spots. High earners in coastal cities are seeing their compensation eroded by housing costs and general expenses that far outpace the national average.
The Gender Pay Gap Widens
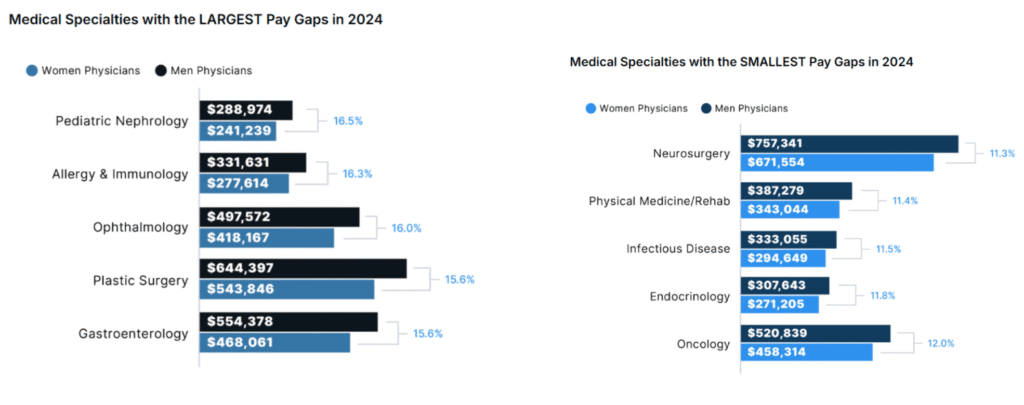
Here’s where the data becomes particularly troubling. The gender pay gap expanded to 26% in 2024, up from 23% the previous year. This represents a full reversal of the modest progress made in 2023.
The disparity stems from dramatically different growth rates. Male physicians saw compensation rise 5.7% in 2024, while female physicians gained just 1.7%. After controlling for specialty, location, and experience, women earned $120,917 less than men on average.
Over a 40-year career, this gap compounds to more than $2 million in lost earnings. For physicians focused on financial independence, this represents years of additional work required to reach the same savings goals as male colleagues.
The gap appears across all specialties examined, exceeding 11% in each field.
Pediatrics: A Systemic Pay Problem
The report exposes what many have long suspected: pediatric medicine faces a compensation crisis. Pediatric specialists earn substantially less than their adult medicine counterparts across every specialty examined, despite similar training requirements and clinical complexity.
The gaps are staggering. Pediatric hematologists and oncologists earn 93% less than adult specialists in the same fields. Pediatric gastroenterologists face an 80% pay differential.
Cardiology, pulmonology, and rheumatology show similar patterns.
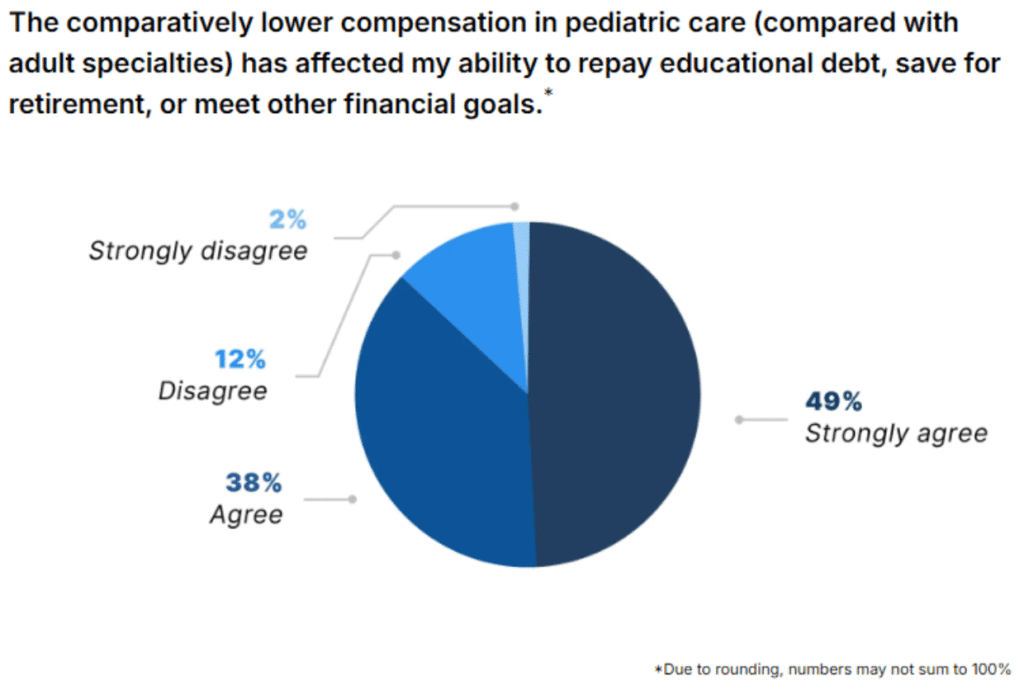
When surveyed, 87% of pediatricians and pediatric subspecialists reported inadequate compensation relative to their work’s complexity and importance.
An equal percentage said lower pay has affected their ability to manage student debt, save for retirement, or meet financial goals. Nearly 69% have considered a career change as a result, with 23% already planning to leave or having left pediatric practice.
The downstream effects appear severe. More than 80% of pediatric physicians reported that the reimbursement gap has worsened recruitment in their field, while 65% said retention has suffered. Half reported that current reimbursement limits their ability to provide care, with another 37% worried it will in the future.
Medicare Reimbursement Pressures
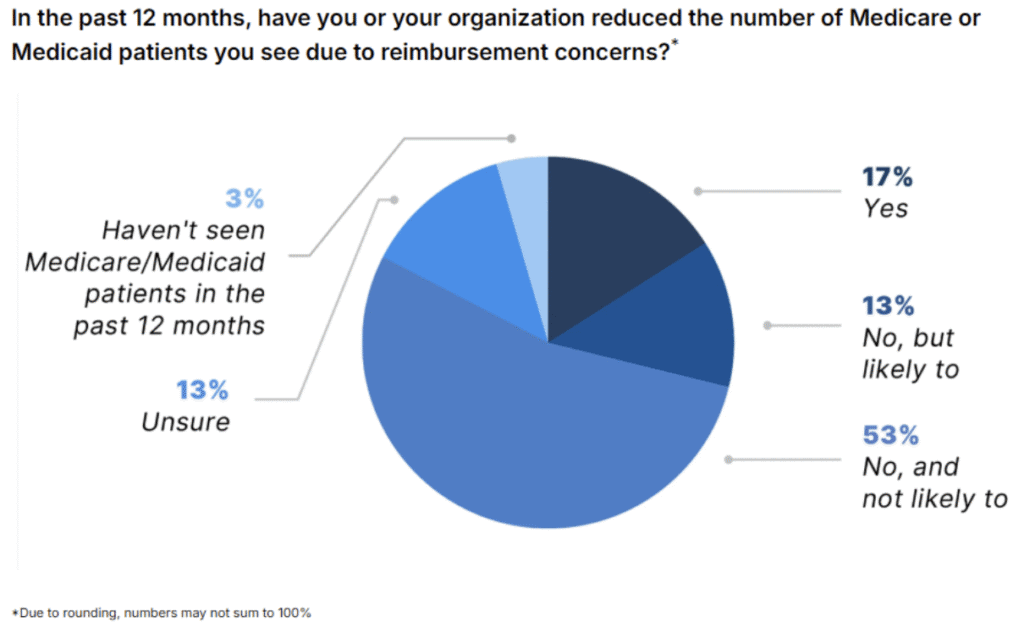
Medicare reimbursement continues its downward trajectory. According to the American Medical Association, Medicare physician payment has dropped 33% since 2001 after adjusting for inflation.
The 2025 schedule includes another 2.8% cut.
Among physicians surveyed, 17% reported reducing the number of Medicare or Medicaid patients seen in the past year due to reimbursement concerns.
Another 13% said they’re likely to do so in the future. While 53% maintained they haven’t made reductions and don’t plan to, 60% expressed concern about their ability to continue serving these populations.
Nearly 38% of physicians reported delaying or canceling plans to hire staff or expand services in the past year due to reimbursement pressures. Another 19% are considering such measures.
The Decline of Private Practice
The data confirms what many have observed: private practice continues its steady decline. Between 2012 and 2024, the percentage of physicians working in private practices fell from 60.1% to 42.2%, an 18-percentage-point drop.
When asked directly, 81% of physicians agreed or strongly agreed that reimbursement policy has played a significant role in this decline. Only 7% disagreed.
For physicians contemplating practice ownership or evaluating employment options, this trend carries clear implications.
The financial pressures that make independent practice increasingly difficult show no signs of abating. The economies of scale and negotiating leverage available to larger health systems create advantages that solo practitioners and small groups struggle to match.
Workforce Strain
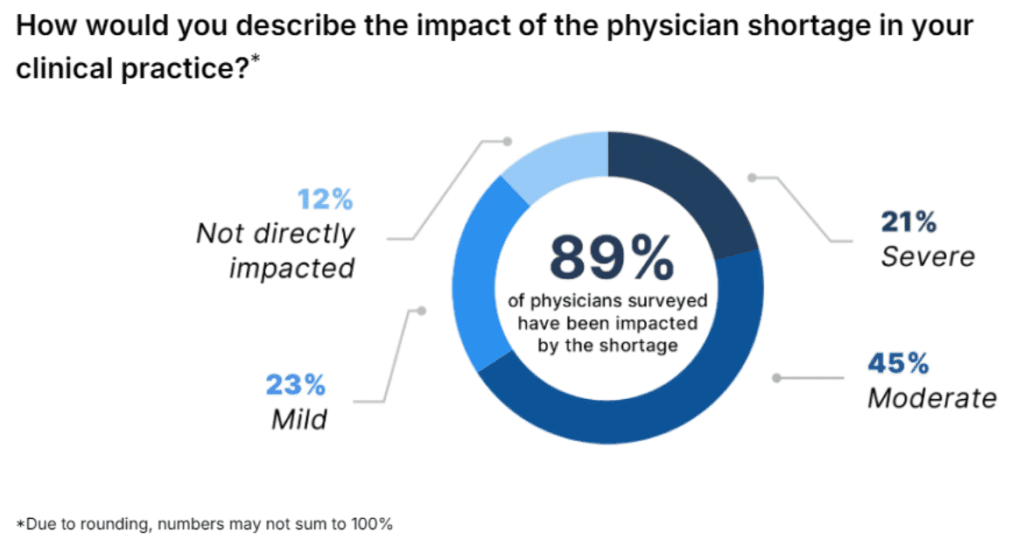
The physician shortage continues to intensify. The Association of American Medical Colleges projects a shortfall of 86,000 physicians by 2036, while the Health Resources and Services Administration estimates an even larger gap of 187,130 full-time equivalent physicians by 2037.
Among surveyed physicians, 89% reported that the shortage has affected their clinical practice, with 21% describing the impact as severe.
The consequences include burnout, overwork, and reduced job satisfaction. Many physicians reported limited or no ability to accept new patients.
The overwork numbers are particularly striking. Eighty-five percent of physicians reported being overworked, up from 81% in 2023. Women physicians reported higher rates of overwork than men (91% versus 80%).
As a result, 68% of physicians said they’re looking for an employment change or considering early retirement.
In response, 77% of physicians said they would accept or have already accepted lower compensation in exchange for greater autonomy or work-life balance.
This represents a slight increase from 75% in 2024 and 71% in 2023.
What This Means for Your Financial Plan
These trends carry several implications for physicians managing their financial trajectories.
First, nominal compensation growth may not translate to real purchasing power gains. With Medicare cuts, inflation effects, and rising practice costs, income growth that appears solid on paper may barely keep pace with expenses.
Second, the gender pay gap requires direct attention. Female physicians should negotiate aggressively, document their productivity and value, and consider geographic moves or practice settings that demonstrate more equitable compensation.
Third, specialty choice continues to drive lifetime earnings substantially. The 93% pay gap between adult and pediatric subspecialists represents millions in lost earning potential over a career.
Private practice also faces structural headwinds unlikely to reverse soon.
Physicians considering ownership should model conservative reimbursement scenarios and understand that compensation premiums from ownership may erode.
Finally, the overwork epidemic suggests many physicians may need to prioritize sustainability over maximum earnings. Seventy-seven percent willing to accept lower pay for better balance indicates a profession reassessing its priorities.
The 2025 compensation landscape offers modest gains on the surface but reveals deeper structural challenges beneath.
Physicians building long-term financial plans would be wise to account for these pressures when projecting future earnings and career paths.









2 thoughts on “Physician Compensation 2025: Modest Gains and Deeper Financial Pressures”
These pressures clearly have long-term implications for workforce sustainability and patient access. Slope
As a physician navigating the evolving landscape of compensation, I found your insights on modest gains versus financial pressures incredibly relevant. The statistics you shared resonate with my experience—despite rising costs across the board, many of us still struggle to maintain our financial health. It’s eye-opening to see how market demands are reshaping our earnings potential.
I’m particularly intrigued by how you highlighted the geometry dash lite disparities in compensation across specialties. Do you think we might see any shifts towards more equitable pay structures in the near future, or is this disparity likely to persist?